Autoimmune Myositis: A closer look into Samantha Ruth Prabhu's disease
- Apr 13, 2023
- 13 min read
Samantha Ruth Prabhu, a renowned South Indian actress, is well known for her work in Telugu and Tamil films and does not need any more introduction. Alongside acting, she is also an entrepreneur, philosopher, and social media activist who frequently campaigned for women’s empowerment. She has a huge fan base all over India.

In an Instagram post last year, she revealed that she had been diagnosed with autoimmune myositis which instantly became a cause of concern for her fans. Despite this, she expressed her gratitude to her followers and reassured them that she is handling, the disease with courage. The actress has been sharing updates about her health now and then. From working on strength in the gym to taking injections, the actress is on a road to recovery from her myositis [1].
Autoimmune myositis is a condition in which the body's immune system attacks the muscles, causing weakness of the muscles. The weakness of the muscles results in difficulty in performing day-to-day activities. This disease gained widespread attention when it was linked to Indian film actress and model Samantha Ruth Prabhu [1].
Read on to learn more about autoimmune myositis.
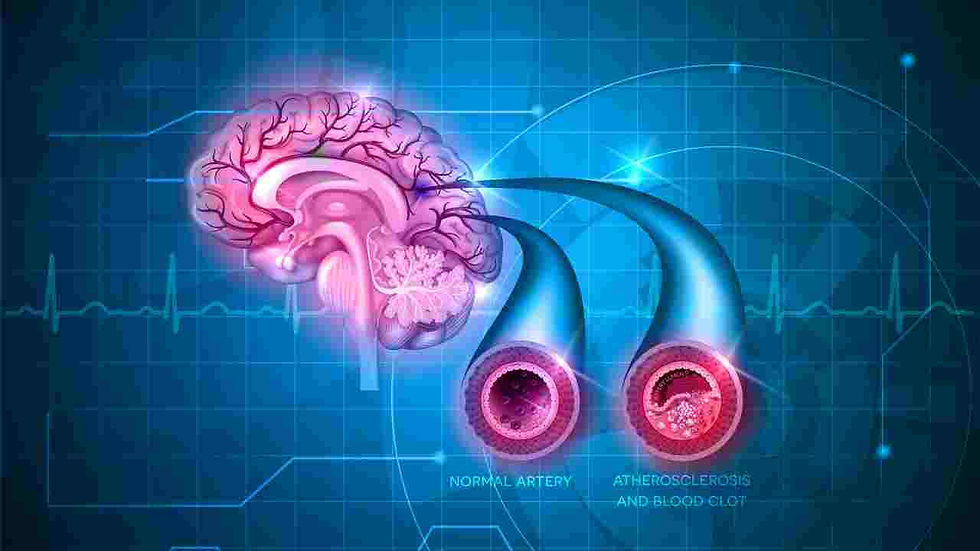
As the name indicates it is a rare autoimmune condition that affects the skeletal muscle system. The body’s immune system attacks the muscle fibers which leads to their inflammation with cardinal signs of rubor (redness), tumor (swelling), calor (increased temperature), dolor (pain), and functio laesa (loss of function) [2]. The clinical features of this condition are as follows:
Autoimmune myositis is a condition that shows bimodal age distribution once at 5 to 15 years and the other at 45 to 60 years. Symptoms are almost similar in both age groups with muscle inflammation (myositis) developing suddenly in children. Features include weakness in the upper arms, hips, and thighs which is symmetrical on both sides, pain in the joints, difficulty with swallowing, fever, fatigue, and weight loss. In some patients, inflammation of the skin is also seen along with the muscle.
The muscles will become rigid and worn out, and frail in autoimmune myositis. Patients also experience severe pain in the muscles. Muscle weakness in autoimmune myositis is so severe that it can cause a sudden fall of a patient while walking or standing and they feel very difficult to stand up after falling. They exhibit greater discomfort in even getting up from a chair. They cannot perform their day-to-day activities and require someone to take care of them.
With reddish-purple swelling around the eyes, a heliotrope rash - also known as a dusky or purplish rash. may develop on the face. The rash can form everywhere on the body, but it is most frequently found on the hands, feet, elbows, knees, outer region of the upper thighs, and knuckles. The skin around the nails may become thicker or redder. Brownish pigmentation, scarring, or pale depigmented regions of skin may appear after the disappearance of the rash [3].
Except for the throat and esophagus, other organ involvement is rarely seen in this myositis. Heart and lungs may be affected, sometimes leading to coughing, shortness of breath, and irregular heart rhythms (arrhythmias). Inflammation of the blood vessels may sometimes lead to gastrointestinal symptoms, which include blood vomiting, black stools, and severe pain with perforation in the lining of the abdominal tract. These symptoms, if exists, are commonly seen in children, but are rare in adults [4].
Autoimmune myositis globally has an estimated prevalence of 5 to 22 per 100,000 people and an annual incidence of 1.2 to 19 per million people. In India, myositis is seen in around 4-22 people per 100,000 lakh population. Myositis is becoming more common as a result of an increase in detection rates. According to the literature, there is not much of a difference in its incidence in blacks and whites, while Hispanics have reported more cases compared to others [5, 6].
Diagnostics
The diagnosis of autoimmune myositis is based on multiple factors such as symptoms, characteristic features, various laboratory blood tests, special radiological investigations, and muscle biopsies.
Laboratory Investigations
The initial blood tests are advised to evaluate the presence or absence of myositis. Muscle weakness which is a prominent feature of myositis may occur either due to muscle problems or nerve damage. The screening tests will help to identify the disease once the symptoms of myositis appear. The initial screening tests are as follows:
Aldolase enzyme test: When the muscle is damaged, the cells release aldolase enzyme into the bloodstream. This helps to identify the origin of muscle weakness which may be due to either muscle or nerve problems. Aldolase enzyme levels will increase in cases of muscle weakness resulting from muscle problems and will not change in case of nerve problems.
Antinuclear antibody (ANA) test: This is a screening blood test to determine an autoimmune disease. An ANA positive test will not however identify a specific disease. Also, a negative ANA test will not rule out myositis.
Creatine Kinase: Creatine Kinase (CK) or Creatine Phosphokinase (CPK) is an important diagnostic blood test for myopathies. The CK enzyme is active in skeletal muscles, heart muscles as well as the brain. When the muscle tissues get damaged, the CK levels are elevated in the bloodstream. CK levels are also often used to evaluate the progress of the disease after treatment.
Erythrocyte Sedimentation Rate: This measures swelling and inflammation of the muscles. This test is not specific to a particular disease but simply identifies the presence and severity of the inflammation. It can be used to watch the progress of muscle inflammation and monitor the effectiveness of the treatment [7].
Imaging
Magnetic resonance imaging (MRI): Magnetic resonance imaging (MRI) is a non-invasive scanning technique that uses a powerful magnetic field and radio waves to generate digital images of organs, soft tissues, bones, and other internal body structures. The level of detail in MRI images allows us to more accurately evaluate these structures to determine the presence of certain factors, such as inflammation, that are related to the disease.
MRI can play an adjunct role in the diagnosis of myositis by identifying the location, distribution, and extension of the disease process. MRI is also useful in presurgical planning by accurately revealing vital information about the proximity of anatomic structures and by identifying fluid collections that may indicate abscesses or tissue necrosis. MRI scans of muscles are especially useful in helping the clinician to identify the best site to perform a muscle biopsy. Hence, MRI is the imaging modality of choice in many cases of myositis.
MRI examination in cases of myositis may reveal diffusely hyperintense T2-weighted signal within affected muscle groups, consistent with muscle edema of myositis. Additional findings include muscle atrophy and fatty replacement which is more severe in patients with anti-SRP antibodies.
Emerging scanning modalities and advancements in MRI for imaging myositis patients are:
P31 magnetic resonance spectroscopy (MRS) has proven to accurately measure intracellular pH in a non-invasive manner.
MR Elastography (MRE). MRE measures tissue stiffness by encoding displacements due to the propagation of externally induced acoustic waves into the MR phase signal [7, 8].
Electrodiagnostic Testing
Electrodiagnostic testing is the core diagnostic modality for patients with suspected myositis. Electrodiagnostic studies are considered an extension of the physical examination and are most useful in the workup of a patient with a suspected myopathy. Electrodiagnostic studies not only allow confirmation of myopathy diagnosis and assist in identifying etiology, but they also can be used for the selection of a suitable site for muscle biopsy or to direct further genetic testing.
It consists of nerve conduction studies (NCS) and electromyography (EMG).
NCS usually precedes EMG and provides valuable information about the function of sensory and motor nerve fibers. NCS is normal in the majority of patients with disorders of muscle and assists in excluding disease mimickers.
Electromyograms are essential to excluding alternative diagnoses and confirming muscle disease when evaluating patients with suspected myopathic disorders. This is helpful to differentiate myositis from nerve disorders. In myositis muscle diseases, the motor neurons are not affected, and in case of a muscle problem, each fiber dies out and is inflamed. If the muscle is affected, then the EMG needle is inserted in the muscle and the patient is asked to contract the muscle; there is a normal response, which indicates an inflammatory response.
EMG is most helpful in determining if muscle weakness and pain are caused by muscle disease or nerve disease. EMG can also help identify the muscle group that is most likely to provide useful information on biopsy. Also, the number of muscles to be tested varies depending on the symptoms [7, 9].
Muscle Biopsy
Muscle biopsy is an invasive procedure preferred, depending on the results of other lab tests. The biopsy is one of the best ways to diagnose myositis and to distinguish it from other muscle disorders. The biopsy specimens are examined by histopathological and immunohistochemistry methods and the features are observed which may lead to a diagnosis of myositis [7, 10].
Myositis specific antibodies
Myositis-specific antibodies: The advanced diagnosis for autoimmune myositis includes the presence of myositis-specific autoantibodies (MSA). These autoantibodies are rarely found in other diseases, so their presence in the patient’s blood can confirm the diagnosis of any form of myositis. Myositis-specific antibodies have also improved the understanding of myositis by leading to the identification of certain clinical patterns that help clinicians understand how the disease might progress.
Other autoantibodies, known as myositis-associated autoantibodies (MAA), have also been identified. These autoantibodies are found in patients with myositis, but they are also present in patients with other autoimmune diseases [7, 11].
Omics
Proteome:
The identification of biological factors important in autoimmune myositis with the help of proteomic profiling would provide clues about the pathophysiological processes and the availability of new reliable markers. Proteomic profiling is used to identify antigen specificities of autoantigens and to identify newer target autoantigens to myositis-specific antibodies [12].
Transcriptome:
In patients with autoimmune myositis, whole-genome transcriptomes of CD4+ and CD8+ T cells from peripheral blood will help to distinguish it from other types of myopathies. The transcriptomic profiles of different subpopulations of T cells in myositis patients could reveal the T-cell phenotypes related to gene expression. To find biomarkers peculiar to certain subtypes of myopathy, transcriptome sequencing (RNAseq) has been used in various cohorts of late-onset muscle disorders [13, 14].
Therapeutics
The current management of autoimmune myositis consists of corticosteroids and immunosuppressive drugs [15]. Initially, the patients are given oral corticosteroids such as prednisolone. This drug does not target the core biology of the disease rather it relieves some of the symptoms by strengthening the muscles, and reducing the pain and swelling. For patients having swallowing difficulties, prednisolone can be given intravenously. The side effects of corticosteroids include high blood sugar levels, mood swings, risk of fractures, and eye problems. Immunosuppressants are also given to reduce inflammation and prevent disease progression. Eventually, the corticosteroids are tapered off and immunosuppressants are continued.

The standard of care therapeutics for the management of autoimmune myositis is the symptomatic treatment of pain and inflammation which does not cure the disease. The management of autoimmune myositis involves specialists in the care of patients, including neurologists, psychiatrists, rheumatologists, pulmonologists, cardiologists, orthopedic surgeons, and others. Thus, the rheumatologist may recommend one of the following advanced therapeutics to improve the quality of life of the patients:
Intravenous immunoglobulins: In this treatment, antibodies obtained from donated blood are injected intravenously into the patient. This prevents the damage caused by the patient’s immune system to their muscles. Particularly, it lowers the rashes and helps with dysphagia (swallowing difficulties). Its safety profile is encouraging and only minor side effects, such as headaches and chills, are reported [15]. One major limitation of this therapy is that the antibodies have to be extracted from thousands of donors to make up a sufficient dose for one patient which makes it extremely expensive. Moreover, it needs to be repeated frequently which increases its cost. Therefore, its use is limited to severe or refractory cases.
Biologics: These are any drugs that are extracted or synthesized from living sources. They include antibodies, toxins, or other proteins. Biologics are being used in the treatment of a variety of disorders. Among various biologics being used in the treatment of autoimmune myositis, rituximab is the most effective. Rituximab is effective in mitigating autoimmune myositis, especially in treating myositis-related interstitial lung disease which is a severe complication of this disease [16]. Other emerging biologics are anakinra, alemtuzumab, belimumab, etanercept, infliximab, tocilizumab, abatacept, and sifalimumab [17, 18].
Physical therapy: Physical exercise is a proven way to improve muscle strength in autoimmune myositis. Patients are encouraged to work closely with a physiotherapist who can design a personalized physical activity plan for them. Physical activity helps patients improve mobility, retain motor function, and prevent the side effects of the above-mentioned medications [19]. Patients can start a strengthening program 2-3 weeks after recovering from an acute phase of the disease.
Stem cell transplantation: Stem cell therapy uses stem cells to repair or replace dysfunctional cells. Stem cells are immature cells that have the potential to develop into different types of cells in the body. Stem cells may be taken from the patient (called autologous stem cell therapy) or from another suitable donor (called allogeneic stem cell therapy). In the case of autoimmune myositis, it can be used to replace the dysfunctional immune cells which have started attacking healthy muscles of the body. Stem cell therapy has been successfully used to increase muscle strength, and induce sustained remission in severe, refractory cases of myositis [20]. However, it can only be used as an add-on treatment and does not provide a cure, and may not be appropriate for all patients.
Gene therapy: It is the application of innovative techniques, such as CRISPR technology, to alter the genetic information stored in cells in the form of DNA. Gene therapy is supported by the rationale that the immune system is attacking the healthy muscles of the body because of some faulty genes and correcting these genes will result in the mitigation of the immune-mediated destruction of muscles. It is still in the early stages of development, and before it can be used clinically to treat autoimmune myositis, it must undergo rigorous safety trials [20].
Quality of life
In the majority of patients, autoimmune myositis significantly affects many domains of quality of life, including functional capacity, psychological or emotional domains, and many other aspects. Even those who are in remission from myositis have a much lower quality of life than the general population. Following are some measures used to improve the quality of life in myositis patients.
1. Physical therapy and exercise
Exercise has recently been recognized as a crucial auxiliary component of treatment for myositis patients. Exercise has been demonstrated to improve muscular metabolism, physical capability, inflammation, fatigue, autonomy, and quality of life in myositis patients. Aerobic exercise has the potential to improve quality of life and muscle function in both patients with recently manifested myositis and those with more advanced diseases.
The suggested exercise methods include cycling, treadmill walking, and resistance training. To increase muscle strength and stop a decline in quality of life, physical activity should be initiated as soon as the patient can able to do it [7, 15].
2. Complementary and self-care therapies
Most people combine traditional or alternative therapies with conventional treatments as a supplementary strategy. Patients should talk to their rheumatologist, neurologist, and/or primary care clinician before starting complementary or unconventional therapies in their treatment regimen. Based on the scientific literature, the Myositis Association makes the following recommendations for complementary therapies [7].
3. Diet and nutrition
Some TMA (The Myositis Association) members have revealed that adopting special diets like paleo or vegan significantly reduces their symptoms. The anti-inflammatory eating plan, often known as the Mediterranean diet, is easily adapted and includes:
Avoid processed and fast foods and choose fresh fruits, vegetables, and unprocessed foods.
Limit intake of bread, pasta, and packaged foods;
Lower consumption of saturated fat (animal fats and palm kernel oil).
Incorporate avocados and nuts, particularly walnuts, cashews, and almonds.
Increase the intake of omega-3 fatty acids.
Consume more vegetarian protein.
Consume chocolate (in moderation) that has at least 70% cocoa.
Along with this, it is advised to take dietary supplements like calcium, vitamin D, folic acid, and omega-3 fatty acids [7].
4. Mind and body practices
Following different methods or techniques are used in mind and body practices, all of which are provided or taught by a qualified practitioner or teacher.
Acupuncture
Chiropractic and osteopathic manipulation
The practices of traditional healers
5. Stress reduction and adequate sleep
High levels of stress and sleep deprivation can exacerbate the symptoms (muscle weakness, discomfort, and skin rashes) in myositis patients. The following strategies can help to manage stress levels.
Massage therapy
Yoga
Relaxation techniques, such as breathing exercises, guided imagery, and progressive muscle relaxation.
Meditation
Prayer
Being in nature and exercising in nature [7]
Those using prednisone may find it particularly difficult to get a good sleep at night. Together with the preceding stress-reduction recommendations, the following sound sleep hygiene tips may be useful.
An hour before going to bed, refrain from watching television, using the computer or playing games, and reading electronic books.
Coffee, caffeinated teas, and chocolate should all be avoided after lunch.
Establish a consistent bedtime regimen that includes regular sleep times.
To fall asleep, listen to music or recordings.
It might be beneficial to occasionally take tryptophan, melatonin, or antihistamines.
Before going to bed, drink warm milk or relaxing herbal tea [7].
6. Self-care practices
Healing depends heavily on taking care of oneself. Myositis patients can practice a variety of self-care tips to maintain their health. Below is a list of a few of these:
Get plenty of rest.
If necessary, take a leave from work.
Maintain and cultivate good relationships.
Have a rewarding or enjoyable element in your life, such as a hobby, close friends, family, or a pet [7].
Clinical trials (Recruiting)
The ongoing recruiting clinical trial currently on autoimmune myositis is as mentioned below: [21]
Title | Intervention | Summary | Location | NCT Number | Date |
Adult Autoimmune Myopathies (MAIA) | Organized collection of longitudinal clinical data and collection of biological samples | This study corresponds to a monocentric prospective cohort of adult patients who are suspected to have an idiopathic inflammatory myopathy. It will enable the creation of both a structured longitudinal clinical data collection and a collection of biological samples, such as blood, urine, stool, and muscle samples. | CHU de BREST Brest, France | NCT04792931 | Start date: May 20, 2022 Completion date: May 20, 2030 |
This blog is to spread awareness and provide accurate detailed information on an extremely rare disease affecting one of India’s top actresses. As part of the Indian audience, we wish Samantha the very best, and a smooth and speedy comeback to acting.
References
[1] “Samantha Prabhu diagnosed with myositis: All about this auto-immune disease,” India Today. https://www.indiatoday.in/health/story/samantha-prabhu-diagnosed-with-myositis-all-about-this-auto-immune-disease-2291474-2022-10-31 (accessed Feb. 24, 2023).
[2] A. Cheeti, L. H. Brent, and S. Panginikkod, “Autoimmune Myopathies,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2022.Accessed: Feb. 24, 2023.[https://pubmed.ncbi.nlm.nih.gov/30422455/]. http://www.ncbi.nlm.nih.gov/books/NBK532860/
[3] I. E. Lundberg et al., “Idiopathic inflammatory myopathies,” Nat Rev Dis Primers, vol. 7, no. 1, p. 86, Dec. 2021, doi: 10.1038/s41572-021-00321-x.
[4] “Autoimmune Myositis - Bone, Joint, and Muscle Disorders,” MSD Manual Consumer Version. https://www.msdmanuals.com/en-in/home/bone,-joint,-and-muscle-disorders/autoimmune-disorders-of-connective-tissue/autoimmune-myositis (accessed Feb. 24, 2023).
[5] Hossain, M. M., Wilkerson, J., McGrath, J. A., Farhadi, P. N., Brokamp, C., Khan, M. T. F., Goldberg, B., Brunner, H. I., Macaluso, M., Miller, F. W., & Rider, L. G. (2022). The Geospatial Distribution of Myositis and Its Phenotypes in the United States and Associations with Roadways: Findings from a National Myositis Patient Registry. Frontiers in Medicine, 9. https://www.frontiersin.org/articles/10.3389/fmed.2022.842586
[6] Valladales-Restrepo, L. F., Delgado-Araujo, A. C., Aristizábal-Carmona, B. S., Saldarriaga-Rivera, L. M., & Machado-Alba, J. E. (2022). Autoimmune Idiopathic Inflammatory Myopathies: Pharmacological Differences and Similarities by Type of Myositis and by Sociodemographic Variables. International Journal of Rheumatology, 2022, e1807571. https://doi.org/10.1155/2022/1807571
[7] https://www.myositis.org/about-myositis/ The Myositis Association.
[8] Paul L. Wasserman, Ashley Way, Saif Baig, and Dheeraj Reddy Gopireddy. “MRI of myositis and other urgent muscle-related disorders”. Emergency Radiology (2021) 28:409–421.
[9] Elena Shanina, Robert G. Smith. Electrodiagnostic Evaluation of Myopathy (2022), http://www.ncbi.nlm.nih.gov/books/NBK564383/
[10] Jon Walters, Atik Baborie. Muscle biopsy: what and why and when? (2020) https://pn.bmj.com/content/20/5/385
[11] Betteridge Z, McHugh N. “Myositis-specific autoantibodies: an important tool to support the diagnosis of myositis” (2016) J Intern Med 2016; 280:8–23.
[12] Gao, S., Luo, H., Zhang, H., Zuo, X., Wang, L., & Zhu, H. (2017). Using multi-omics methods to understand dermatomyositis/polymyositis. Autoimmunity Reviews, 16(10), 1044-1048.
[13] Joel, M. M., Pontifex, C., Martens, K., Chhibber, S., de Koning, J., & Pfeffer, G. (2022). Transcriptome analysis from muscle biopsy tissues in late-onset myopathies identifies potential biomarkers correlating to muscle pathology. Neuromuscular Disorders, 32(8), 643-653.
[14] Houtman, M., Ekholm, L., Hesselberg, E., Chemin, K., Malmström, V., Reed, A. M., & Padyukov, L. (2018). T-cell transcriptomics from peripheral blood highlights differences between polymyositis and dermatomyositis patients. Arthritis research & therapy, 20, 1-15.









Comments